
Novel Neurostimulation Treatment for Swallowing Disorders – Optimising the Brain’s Power in Rehabilitation
It is a blissful late summer afternoon. The sun is shining, birds are chirping, the sky is clear and a gentle breeze is blowing. You are sitting in a Biergarten, and your friend has just proposed a toast to celebrate this wonderful day. You take a sip of your favourite beer. However, as you swallow the beer, you suddenly start to cough uncontrollably. You can feel that the beer has gone down the wrong pipe. Your heart is beating fast and your face turns red, partly from the vigorous coughing and partly from the embarrassment. You cannot breathe properly because you cannot stop coughing for 10 minutes.
You have probably had a similar experience at least once in your life. However, this is what people with swallowing disorders go through on a daily basis. Swallowing disorders are a common problem among patients with neurological disorders or among elderly people. The consequences of swallowing disorders can be devastating, affecting not only the physical health but also one’s mental well-being. Speech therapists play a crucial role in helping these patients restore their swallowing ability and swallow safely, but not all patients respond well to swallowing treatments.
What Happens During Swallowing and What Happens When It Goes Wrong?
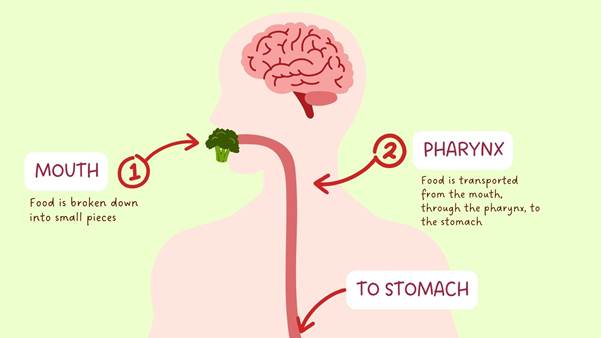
Swallowing is one of the most primitive functions of human beings and we start to develop swallowing skills in the womb at the age of 15 weeks. It is a complicated process where food is transported from the mouth, through the pharynx (the throat) and the oesophagus, and all the way into the stomach (Figure 1). This process involves over 25 pairs of muscles and nerves but takes only 1-2 seconds in a healthy adult.
A normal swallowing process can be divided into three stages: The first stage is the oral preparatory and transit stage, where food is broken down into smaller pieces and mixed with saliva, then pushed from the front to the back of the mouth. Once the food reaches the back of the mouth, it triggers the swallowing reflex, marking the beginning of the second stage of swallowing, the pharyngeal stage. During this stage, a series of protective mechanisms are activated to ensure that the food travels down the oesophagus and not down the windpipe. Finally, the food passes through the oesophagus and reaches the stomach, marking the end of the final stage, the oesophageal stage. This entire process is controlled by the brain.
Damage to the brain can lead to disruptions in this process, resulting in swallowing difficulties, also known as dysphagia. In elderly people or in individuals with neurological conditions such as stroke, Parkinson’s disease or amyotrophic lateral sclerosis (ALS), the ability to coordinate various muscles that are required to pass the food safely and efficiently may be compromised. As a result, they may experience choking, coughing and the sensation of food being stuck in their throat when they drink or eat. When the food accidentally gets into the windpipe, it may cause a chest infection or aspiration pneumonia. Besides, dysphagia can also cause long-term complications such as malnutrition, dehydration or even death. Many patients with dysphagia feel embarrassed and anxious during mealtimes so that they may avoid mealtimes with their family and friends, which negatively affects their psychosocial wellbeing and their quality of life.
What Kind of Treatments Can Help Them Swallow Safely and What Are Their Limitations?
Speech therapists play an important role in helping these patients swallow efficiently and safely. Traditional treatments may include changing the texture of food and drinks, changing the patients’ eating posture, and exercises targeting the muscles involved in swallowing. While these treatments may help some patients, there are still many who do not benefit from them or experience only limited improvement. So, how does one help these patients? Let’s learn about the latest developments in swallowing treatments and how they can help these patients.
Neuroplasticity – The Key to Recovering the Swallowing Function
Before delving into the latest developments in swallowing treatments, let’s look at a key concept in rehabilitation — “neuroplasticity”. Neuroplasticity is a mechanism by which the brain reorganizes itself after an injury. Imagine a river stream flowing down from a mountain. If you place a large rock in the middle of the stream, the water will not stop flowing, instead it will flow around the edge of the rock, forming new streams and continuing to travel down the mountain. A similar reorganisation takes place in the brain after it is injured, for example after a stroke or a brain injury. Within the first few days to weeks after the injury, a reorganisation of the brain’s neural network takes place: The brain can form new neural connections that take over the function of the damaged parts of the brain.
Novel treatment – The Role of Neurostimulation in Dysphagia Rehabilitation and The Challenges
Over the past two decades, researchers have found that neurostimulation techniques can potentially benefit patients with dysphagia. These techniques aim to promote neuroplasticity by stimulating the nervous system, which ultimately boosts the recovery of the swallowing function.
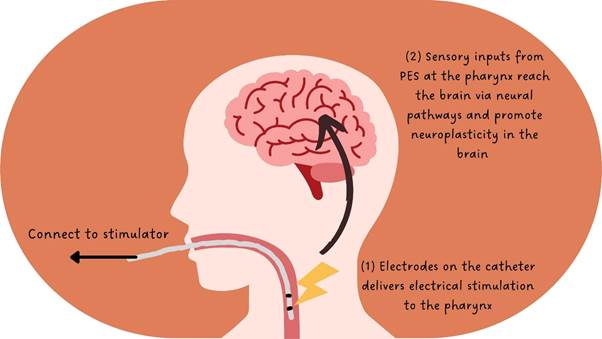
Neurostimulation can be delivered to the peripheral muscles or to the brain. Pharyngeal electrical stimulation (PES) is a form of peripheral neurostimulation. During PES, an electrical current is delivered to the pharynx through a catheter that passes from the nose or mouth to the pharynx (Figure 2). This stimulation increases the sensory input from the pharynx to the brain, which promotes neuroplasticity and facilitates the functional recovery in patients with dysphagia after a stroke.
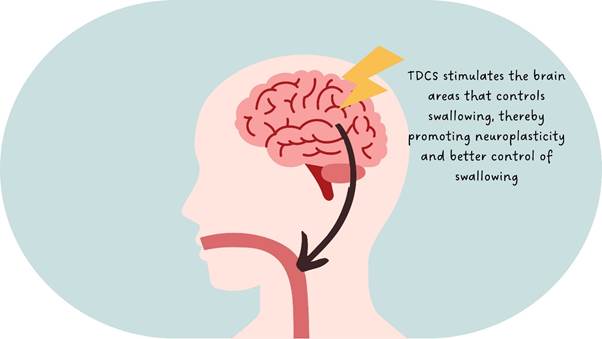
Transcranial direct current stimulation (tDCS) is another form of neurostimulation. Similar to PES, tDCS uses an electrical current to stimulate the nervous system. However, unlike PES, tDCS stimulates the brain regions that control the act of swallowing. TDCS is a non-invasive brain stimulation technique because it does not require surgical procedures to stimulate the brain. During tDCS, electrodes are placed over the scalp to deliver the electrical current (Figure 3). The current penetrates through the skull and acts on the brain cells underneath, thereby subtly regulating the brain activities. When applied to the brain areas that control swallowing, tDCS can promote neuroplasticity and help stroke patients restore their swallowing functions (Figure 4).

The benefits of these neurostimulation techniques have been extensively investigated in many physiological studies in healthy adults and in patients with neurogenic dysphagia. However, there is a small subset of patients who do not respond well to these treatments. Recently, scientists have discovered that the response to neurostimulation may be related to the brain activity prior to treatment.
Metaplasticity – “The Plasticity of Neuroplasticity”
This brings us to the concept of “metaplasticity”. Metaplasticity is a homeostatic mechanism of the brain, and it has been described as the “plasticity of neuroplasticity”. It means that the brain can adjust its capacity to respond to neuroplasticity changes. In other words, the extent to which the brain reorganizes itself depends on the state of the brain.
Neuroplasticity changes can take place in the form of enhanced or reduced brain activity. Excitatory neurostimulation such as PES and anodal tDCS, can increase brain activity and transform the stimulated part of the brain into an excited state. In contrast, inhibitory neurostimulation decreases brain activity, turning the brain into a suppressed state. When the brain is in an excited state, it becomes less receptive to further excitatory stimulation and more receptive to inhibitory stimulation to avoid over-excitation of nerve cells. Conversely, when the brain is in a suppressed state, it becomes less receptive to further inhibition and more receptive to excitatory stimulation.
How can Metaplasticity Mechanisms Improve the Outcomes of Neurostimulation Treatments and What’s Next?
My current research focuses on utilising this mechanism to develop strategies that can minimise the variability in the patients’ response to neurostimulation treatments so that more patients can benefit from them. Our research team in Prof. Suntrup-Krüger’s lab at the University of Münster is conducting a randomised controlled trial study to investigate whether the combined application of tDCS with PES is better than the use of PES alone in improving swallowing functions. We hypothesize that tDCS can be used to condition the brain into a certain state, making it more receptive to the subsequent treatment, that is, PES.
Although the use of neurostimulation for dysphagia rehabilitation holds great promise, further research is needed to optimize its application. Factors such as optimal stimulation parameters, individualised treatment protocols and long-term effects still need to be thoroughly investigated. Future large-scale clinical trials in different patient populations are essential to address these issues.
Do you want to know more about what neurostimulation research can achieve? To gain more insight into how tDCS is being used in research, check out another blog post by one of our former fellows, Dr. Nieves Fuentes Sánchez, whose research focuses on modulating people’s emotional reactions to music.
